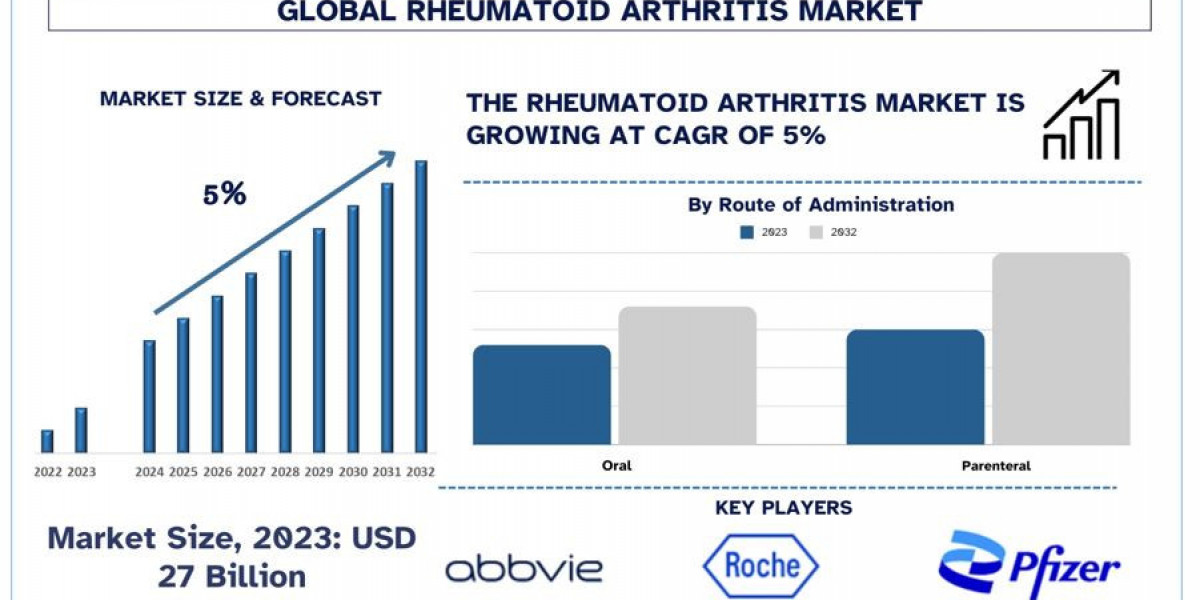
According to a new report by UnivDatos Market Insights, the Rheumatoid Arthritis Market is expected to reach USD 41 Billion in 2032 by growing at a CAGR of ~5%. Rheumatoid Arthritis (RA) is a chronic inflammatory disorder primarily affecting joints, leading to painful swelling, stiffness, and potential joint deformity and erosion. It is an autoimmune condition where the immune system mistakenly attacks the body's tissues. RA can also affect other systems, including the skin, eyes, lungs, heart, and blood vessels. This disease predominantly impacts individuals between the ages of 30 and 60, with women being more commonly affected than men. The exact cause of RA is not fully understood, but it is believed to result from a combination of genetic and environmental factors. Specific genes may increase the risk, and triggers such as infections or hormonal changes may contribute to the disease onset. Smoking and obesity are known risk factors that can exacerbate the condition.
The prevalence of RA is increasing with the aging global population. As people live longer, the incidence of age-related conditions, including autoimmune diseases like RA, rises. For instance, as per the data of Census.gov, The number of Americans aged 65 and older is projected to increase from 58 million in 2022 to 82 million by 2050, representing a 47% increase. This age group’s share of the total population is also expected to rise from 17% to 23% by 2050.
Request To Download Sample of This Strategic Report - https://univdatos.com/get-a-free-sample-form-php/?product_id=63184
Therapeutic Landscape of Rheumatoid Arthritis
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are frequently used to treat RA-related pain and inflammation. They relieve symptoms, but they don't change how the illness progresses. Naproxen and ibuprofen are two examples. Long-term use is linked to adverse consequences related to the kidneys, heart, and gastrointestinal tract, despite the medication's effectiveness in managing pain.
2. Corticosteroids
Strong anti-inflammatory drugs called corticosteroids, including prednisone, are used to rapidly manage acute RA flare-ups. They can be injected intravenously, intra-articularly, or orally. Due to possible side effects such as osteoporosis, hypertension, and an increased risk of infection, long-term use is restricted.
3. Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are the cornerstone of RA treatment, aimed at slowing disease progression and preventing joint damage.
Conventional Synthetic DMARDs (csDMARDs): These include methotrexate, sulfasalazine, leflunomide, and hydroxychloroquine. Methotrexate is often the first-line treatment and can be used alone or in combination with other DMARDs.
Biologic DMARDs (bDMARDs): These are targeted therapies that inhibit specific components of the immune system. They include:
TNF Inhibitors: Examples are etanercept, infliximab, and adalimumab. These drugs block tumor necrosis factor (TNF), a pro-inflammatory cytokine involved in RA pathogenesis.
IL-6 Inhibitors: Tocilizumab and sarilumab inhibit interleukin-6, another cytokine that contributes to inflammation.
B-Cell Depletion Therapy: Rituximab targets CD20 on B-cells, reducing their role in the autoimmune response.
T-cell Costimulation Blockers: Abatacept inhibits the activation of T-cells, which play a critical role in the autoimmune process.
Targeted Synthetic DMARDs (tsDMARDs): These include Janus kinase (JAK) inhibitors such as tofacitinib, baricitinib, and upadacitinib. They interfere with intracellular signaling pathways involved in immune cell activation and cytokine production.
4. Combination Therapy
Combining DMARDs, often with methotrexate as the anchor drug, can enhance therapeutic efficacy. This approach can involve csDMARDs, bDMARDs, or tsDMARDs in various combinations tailored to the patient's disease severity and response to treatment.
5. Non-Pharmacologic Therapies
In addition to pharmacologic treatments, non-drug therapies play a vital role in managing RA. These include physical therapy, occupational therapy, exercise, and lifestyle modifications such as smoking cessation and weight management. These interventions help maintain joint function, reduce pain, and improve overall health.
6. Emerging Therapies
The RA therapeutic landscape continues to evolve with ongoing research and development. Novel agents targeting different pathways in the immune response and personalized medicine approaches are under investigation. Advances in biomarker research aim to identify patients likely to benefit from specific therapies, enhancing treatment precision and efficacy.
Ask for Report Customization - https://univdatos.com/get-a-free-sample-form-php/?product_id=63184
Conclusion
In conclusion, the therapeutic landscape for rheumatoid arthritis (RA) has greatly evolved, offering a wide range of treatments aimed at managing symptoms, preventing joint damage, and enhancing patients' quality of life. From NSAIDs and corticosteroids to conventional synthetic and biologic DMARDs, the options for RA treatment are diverse and continually expanding. Advances in targeted therapies like JAK inhibitors, along with a multidisciplinary approach that includes non-pharmacologic interventions, underscore the importance of personalized and comprehensive care in effectively managing this chronic autoimmune disease. Ongoing research and innovation promise further improvements in RA treatment and patient outcomes.